Business
Parents of Premature Babies Fight for the Support Their Children Deserve
JOLIET, Ill. — After enduring several stressful months in the neonatal intensive care unit, Karen Heath eagerly anticipated taking her triplet sons home. Born at just 25 weeks, each baby weighed over a pound and faced grim survival odds. Thankfully, the boys defied expectations. However, Heath had to wait three months before she could hold them, relying instead on photos and blown kisses.
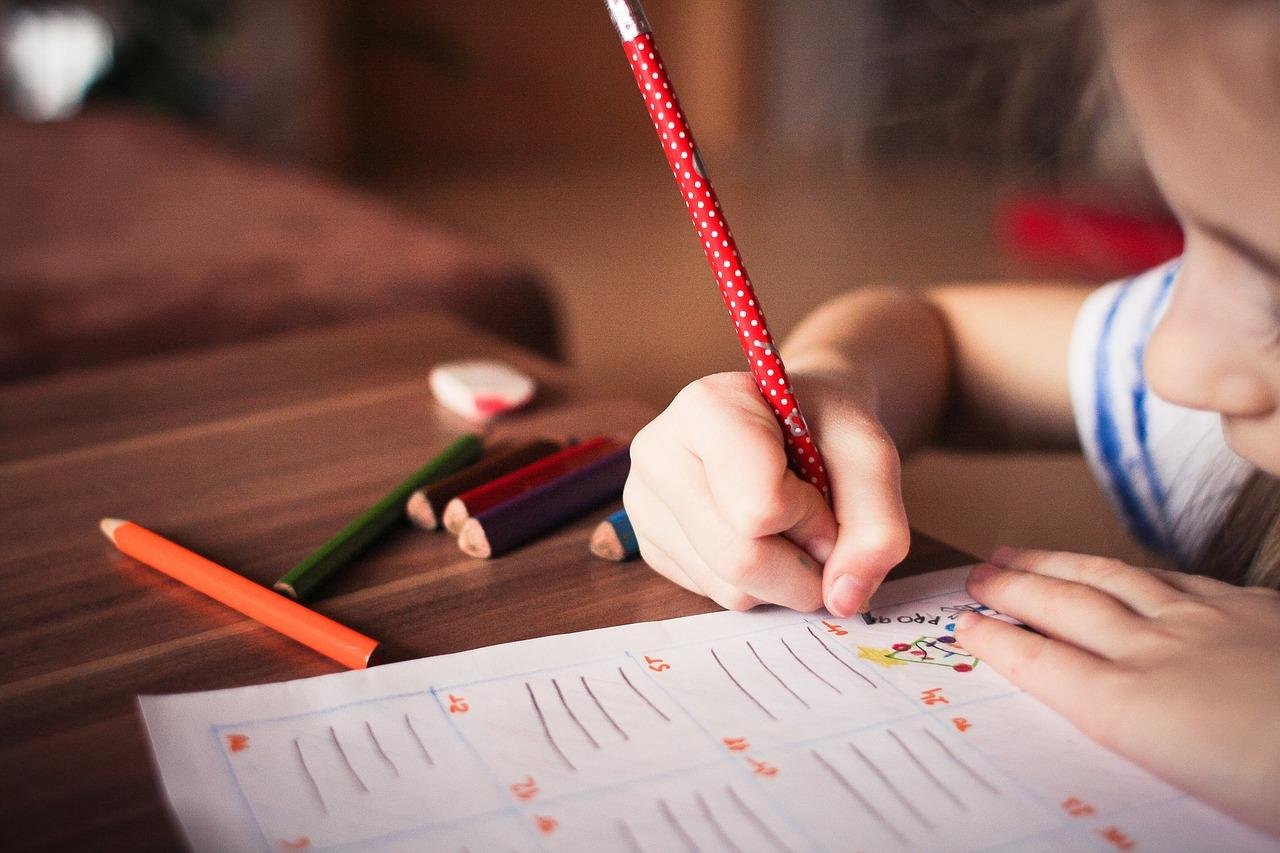
The discharge in early summer 2019 was joyous yet hurried. A physical therapist briefly taught Heath exercises to strengthen the babies, while a nurse provided a crash course on using the oxygen tanks required for their first few months at home. Amidst gathering essentials like diapers and hospital bands, Heath realized a vital piece of advice was missing: her sons were automatically eligible for early intervention services, which include various therapies essential for their development.
“This should have been a conversation well before the boys’ release,” said Heath. Progress in saving the lives of extremely premature infants has surged; survival rates have soared from 5% in the 1960s to around 90% today. Despite this success, access to follow-up therapies remains inadequate across the nation, particularly for families leaving the NICU.
Studies show that children who receive early intervention are less likely to require special education services as they grow. Yet in Illinois, systemic failures hinder access. “We have so much information on early brain development now,” noted Alison Liddle, a physical therapist involved in Chicago studies. Parents struggle to navigate the convoluted systems designed to support them. “Support systems need to catch up. We have a critical window to help families,” she emphasized.
Under federal law, newborns with developmental delays can access early intervention services from birth to age 3. However, state-level differences in program design and eligibility criteria leave many infants without adequate support. Alarmingly, just 1% of infants and toddlers under 1 receive the therapies they need, despite an estimated 13% qualifying.
This disparity in early intervention access echoes broader societal issues. Dr. Michael Msall, a neurodevelopmental pediatrician, likened the situation to people learning of Social Security eligibility too late. Parents face high stakes: timely therapy can mitigate future complications and developmental delays.
Communication is often the biggest hurdle. Misunderstandings can occur even when therapists provide instruction, leading to missed opportunities for necessary services. “They really put the onus on families to secure better outcomes,” said Jaclyn Vasquez, who has personal experience with a NICU stay.
In Illinois, the Legislative Black Caucus previously urged for demonstration projects aimed at enhancing connections between NICU families and available services. Despite legislative support, the initiative lacked funding and has yet to materialize. Meanwhile, a coalition of therapists and hospital physicians has been examining barriers families face after NICU discharge.
Their study revealed only 13% of eligible families were receiving early intervention services three to four months post-discharge. Complicated bureaucracy and poor communication were the main culprits, according to researchers. “When the system is difficult to navigate, families give up,” Liddle remarked.
By June 2019, Heath’s triplets were back at home, but challenges persisted. It took weeks for the family to get a referral for early intervention despite automatic eligibility due to low birth weight. By the time therapy began, it was early 2020, and the pandemic posed additional challenges to accessing in-person services.
Families participating in a pilot study already faced hurdles, even with early intervention plans in place. Accessibility issues, including caseload overloads and outdated communication methods among coordinators, further complicated matters. The Illinois early intervention system has been criticized for systemic inequities, particularly affecting lower-income families and communities of color.
Liddle noted that confusion about eligibility criteria could result in families being wrongfully denied services. These discrepancies vary by state, causing additional frustration. Communication breakdowns between medical and intervention systems further hinder access to timely support.
In contrast, Vasquez’s experience as a special education teacher equipped her to seek help immediately for her premature daughter. This proactive approach allowed her child to access multiple therapies shortly after coming home. As a result, her daughter is currently thriving, reversing dire predictions made about her development.
Healthcare professionals and advocates agree that families should not have to wait until NICU discharge to begin accessing services. Recommendations include embedding early intervention staff in hospitals to streamline connections to therapy. “We dream of having families enrolled before they go home,” said Dr. Raye-Ann deRegnier, who leads related studies.
Advocates in Illinois are hopeful for new funding opportunities to promote pilot programs in NICUs, which could lead to necessary systemic reform. Until then, countless families like Heath’s continue to navigate a flawed system, often left to fend for themselves in securing critical interventions for their children.
Despite numerous obstacles, Heath’s triplets have made significant progress. Now in kindergarten, they bravely don Spider-Man costumes, displaying their playful spirit. Amidst the challenges, Heath remains grateful for the growth her sons have achieved, yet she reflects on the gap in support they encountered during their earliest days. “There was no next step for my family when we left the hospital. It was all on us,” she says, highlighting the need for substantial improvements in early intervention support.